Phage Therapy in the UK and Other Countries
In this second article about phage therapy, I will be focussing on its use in different countries, with special emphasis on the UK.
Phage Therapy in the UK
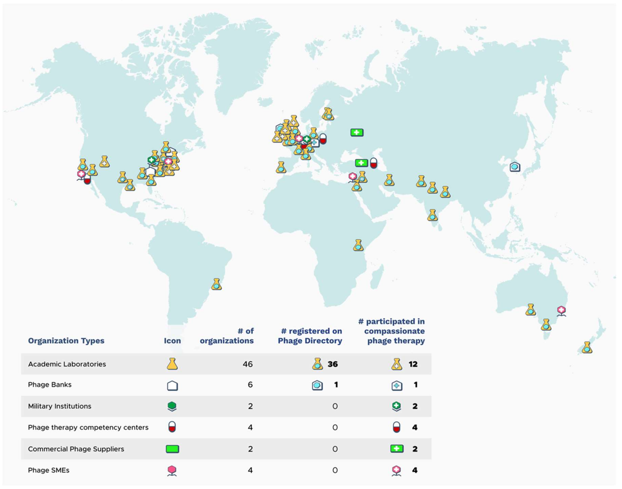
In the UK, phages are classed as a biological medicine and none are licensed for clinical use. As a result, phage therapy is applied on a compassionate use basis as an unlicensed medicinal product (a “special”). Phages imported for use as an unlicensed medicine in the UK do not need to be manufactured according to Good Manufacturing Practice (GMP), however, the Medicines and Healthcare products Regulatory Agency (MHRA) must be notified at least 28 days prior to importation, and doses imported are limited to a small number. Paradoxically, phages manufactured in the UK must be produced to GMP, including phage for use in clinical trials. As a result, the current clinical provision of phage therapy in the UK is ad hoc and relies heavily upon networking with international sources of phages, including organisations such as Phage Directory, who help connect clinicians who want phages for clinical use, with groups who have appropriate phages. The MHRA recently published a document on the regulatory considerations for therapeutic use of bacteriophages in the UK.
According to Phage-UK there have been 24 clinical trials involving phage therapy since 2020.
Phage Therapy in Other Countries
Globally, different countries have different regulatory frameworks for the clinical use of phage therapy.
Eastern European countries have over 100 years of phage therapy experience. Russia and Ukraine allow open use and commercialisation of phage products. Phages are a standard medical application in Georgia. In Poland, specialised institutes have supplied personalised phage products to physicians since 2005.
In the European Union (EU), phage therapy is not approved as a standard medicinal product for human use. Like the UK, It is primarily used in compassionate use cases, clinical trials, or for individual experimental therapy attempts. Although a European Medicines Agency (EMA) guideline exists for veterinary bacteriophage medicinal products, there is currently no corresponding regulatory guidance for human use of such products in the EU. The EMA opened a public consultation on a concept paper on the development and manufacture guidelines for human bacteriophage medicinal products tailored to phage therapy on 23rd December 2023, which ended on 31st March 2024. In the meantime, a regulatory roadmap for phage therapy under EU pharmaceutical legislation has been published.
Belgium has implemented a phage therapy framework focusing on magistral phage preparations that allows patients to actively seek access to personalized phage therapy. In the magistral approach, individual phages are prepared according to a phage monograph (a standardized document that provides detailed information about a specific bacteriophage, its properties, and its potential use in phage therapy), and reference laboratories provide quality control (QC) testing. Clinicians prescribe phage cocktail preparations for use in specific patients, which are then prepared by pharmacists. Based on the Belgian model, a general chapter on phage therapy medicinal products was published in 2024 by the European Pharmacopeia.
In Australia, all clinicians and researchers within the Phage Australia network have adopted the Standardised Treatment and Monitoring Protocol for Adults and Paediatric Patients (STAMP). STAMP is a clinical protocol for administering and monitoring phage therapy, rather than the phage product. As a result, STAMP looks at the process, not the product and means that different patients can be treated with different phages at different sites of infection, but the treatment protocol is standardised. The STAMP protocol has been approved by Australia's national ethics committee and endorsed by Australia's national infectious disease physician society, as well as its paediatric arm.
In the US, phage therapy is not yet an FDA licensed treatment. However, it available under a special programme called the “expanded access eIND system”. For patients who have exhausted standard-of-care therapy, an application is submitted to the FDA by the treating physician, where a patient meets a list of criteria. UC San Diego's IPATH is the first dedicated phage therapy centre in North America. They focus on treating patients with life-threatening multi-drug resistant infections through the FDA's compassionate use program. IPATH also works to advance phage therapy into clinical trials and provides guidance to physicians worldwide on phage therapy protocols. The PhagesDB database details over 25,000 new phages identified by the SEA-PHAGES programme at the University of Pittsburgh. One particular phage from this collection, called Muddy, has been used therapeutically in a cystic fibrosis patient infected with a multi-drug resistant strain of Mycobacterium abscessus. Creative Biolabs is developing libraries of characterised phages, as sell as platforms for identifying and then producing phages to GMP standard for formulation and delivery.
Israel focusses on compassionate use of phage therapy, with the Israeli Phage Therapy Center conducting all of the steps required, from phage isolation and characterization to treatments for non-resolving bacterial infections.
In India, phage therapy is offered as compassionate Phage Therapy regulated by the Declaration of Helsinki and coordinated by the Central Drugs Standard Control Organization. Vitalis Phage Therapy has created a framework for patients to access phage therapy in India.
In China, there are two routes to using phage therapy applications. Phage products with fixed ingredients are regulated as innovative biological products. Personalized phage therapies, on the other hand, need to go through investigator-initiated trials (IIT) and, if successful, the phage therapeutic can then be used at certain institutions.
Expanding the Use of Phage Therapy in the UK
To progress past the ad hoc use of phage therapy in the UK, the infrastructure to support the route from patient enrolment, through isolation and identification of pathogenic bacteria and therapeutic phages, to formulation, administration and monitoring of efficacy, as well as phage resistance, will need to be put in place. A key requirement for clinicians in the UK will be the ability to access phages that are efficient at killing the strain of bacteria causing an infection. A roadmap for the delivery of clinical phage therapy to the UK has been proposed, which would require: expansion of existing phage biobanks; the development of both personalised treatments for individual patients; and off-the-shelf phage cocktails that could be used to treat large numbers of patients.
Innovate UK has developed the Phage Innovation Network to help drive the use of phage based therapy in the UK and build on the expertise of the many phage experts based in the UK. To enable this, systematic librariesof a diverse array of phages that are well characterised and curated, as well as manufactured to GMP standard will be needed.
The Citizen Phage group at Exeter University, uses volunteer citizen scientists to collect samples from a wide range of environments to facilitate the laboratory identification of new phages for therapeutic use.
The UK Phage Library at the University of Leicester is aiming to develop libraries of phages which can be screened against specific bacterial strains to identify phages they are sensitive to. Unfortunately, these phages cannot be used in patients in the UK due to lack of GMP phage manufacturing capability, but they are provided for use in other countries whose regulatory frameworks permit their use.
On the commercial side, Nexabiome in Glasgow aims to provide an end-to-end service covering phage identification and isolation, to production and formulation.
Establishing a UK Phage Manufacturing Facility that can produce phage preparations for both commercial and non-commercial customers that are suitable for administering to patients would be a key requirement for widening the use of phage therapy in the UK. Towards this end, UK Phage Therapy is working with public and private partners to establish a centralised phage susceptibility testing and GMP phage production facility in the UK via the Centre for Process Innovation (CPI). The Centre for Phage Research is also working with regulators, policymakers and other stakeholders to establish frameworks and pathways to enable public access to phage products. Whether the UK will remove the requirement for GMP manufacture of phages for Phase I clinical trials, as is the case in the US, is unclear. However, phase II/III trials would still require GMP manufacture for off-the-shelf phage products.
Phage-UK has developed a standardised protocol for the treatment and monitoring of phage therapy in UK patients suffering from cystic fibrosis and bronchiectasis, where there is no alternative treatment available. The protocol, based upon the Australian STAMP protocol, is a document that assists clinicians making a submission to their NHS Hospital Board for approval to use phage therapy on a named patient basis. Presumably, this protocol could be adapted for the treatment of UK patients with other serious infections such as urinary tract infections (UTIs), prosthetic joint infections (PJIs) and sepsis. A benefit of using such a standardised protocol would be the collection of safety and efficacy data on phage therapy that could then inform the design of subsequent clinical trials of phage therapy in the UK.
Conclusion
For most countries, compassionate use is the major pathway for patients to access phage therapy. Belgium (with the magistral approach), and Australia (with STAMP), currently lead the way in developing frameworks to facilitate patient access to phage therapy. The lack of such frameworks in other countries, including the UK, reflect the view that phage therapy is still an experimental treatment that requires more convincing clinical evidence of efficacy. In the UK, it will be interesting to see if any of the recommendations made in the March 2024 Policy Paper on the antimicrobial potential of bacteriophages, published under the Conservative government in power at the time, are followed up by the current Labour government.